The Late-Night Prenatal Test – The Overlooked Folate Crisis
"Your fetus has double the normal risk of neural tube defects," the obstetrics clinic lights reflecting on Jessica's trembling hands. With a BMI of 34.5, she had been dutifully taking folic acid supplements daily since preconception, her diet brimming with spinach salads and avocado smoothies. Yet, despite normal serum folate levels, why was the risk alarm still blaring?

This paradox is surprisingly common among overweight pregnant women.
A study from the University of Colorado tracked 24 women at 8-22 weeks of gestation and found:
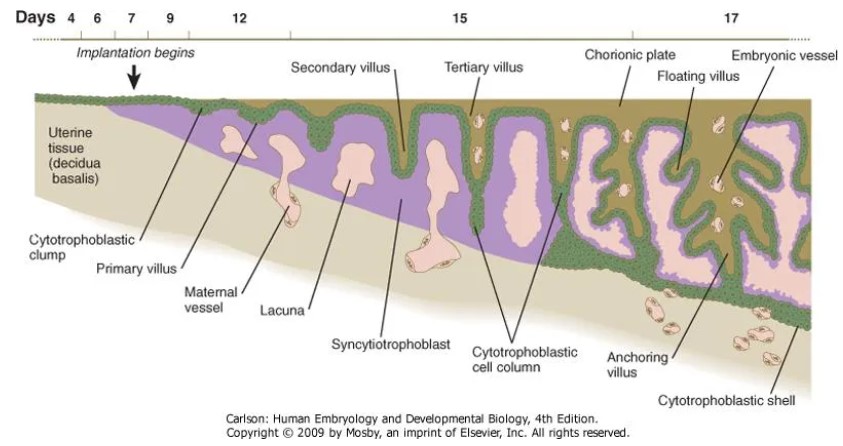
While the placenta in normal-weight mothers efficiently transports folate, in the high-BMI group, the expression of key transport proteins RFC (reduced folate carrier) and FR-α (folate receptor α) on the microvillous membrane (MVM) of the placenta, the critical site for nutrient exchange, plummeted by 19% and 17%, respectively. Folate transport efficiency dropped a staggering 52%.
It's akin to having a leaky sieve in the fetus's "nutrient warehouse." Even with ample maternal folate reserves, the fetus may still experience "hidden hunger."

The Placental Transport Black Box – How Overweight Chokes Folate Channels?
1. The Sugar-Coated Transport Hub
The syncytiotrophoblast layer of the placenta resembles a precision customs system, with RFC and FR-α as the "transport fleet" shuttling through the MVM.
However, in overweight mothers, hyperinsulinemia and chronic inflammation are like smearing sticky syrup on these "trucks."
Research confirms that in the high-BMI group, the activity of folate transport proteins in the placental MVM is significantly reduced. Surprisingly, it's not the regulatory system (mTOR signaling pathway, the "switch" for cell growth) that's at fault, but rather the transport tools themselves are "corroded."
2. The Critical 72 Hours
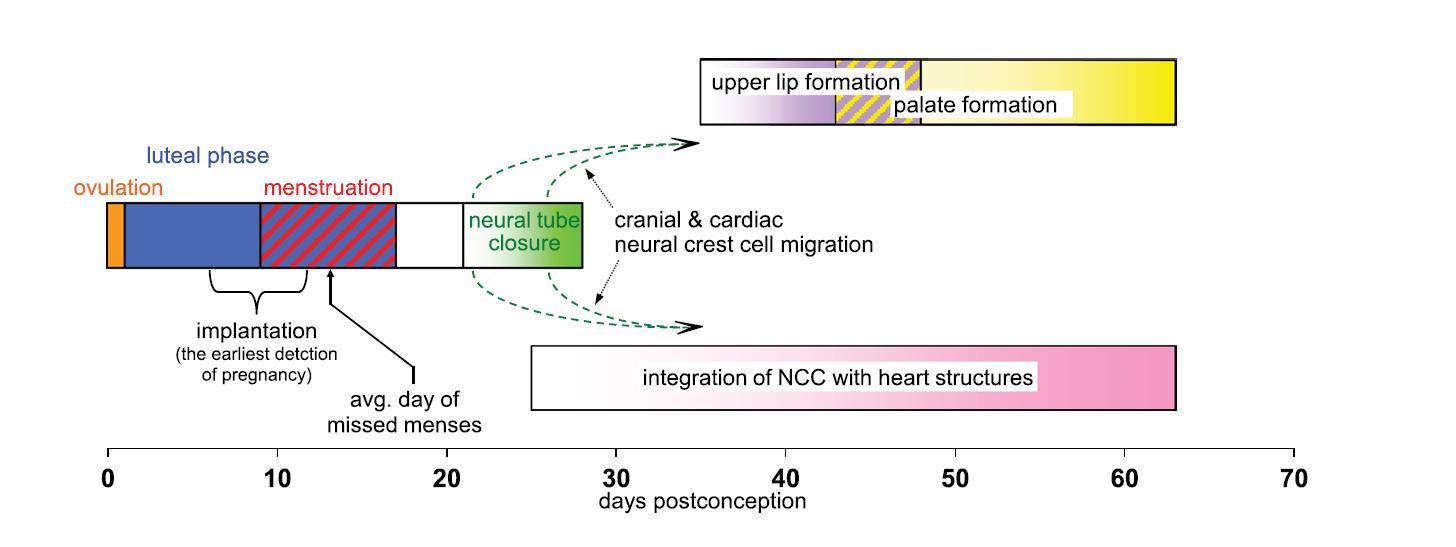
Neural tube closure occurs between 21-28 days of gestation. Even minor differences in placental transport efficiency during this window can spell disaster.
Ordinary folic acid (synthetic folic acid) must be converted into 6S-5-methyltetrahydrofolate (active folate) to be absorbed. However, overweight mothers may already have reduced metabolic enzyme activity. This "secondary conversion" is akin to adding another valve to an already clogged pipeline.
It's like trying to charge a dying phone with a poor-quality cable – it seems to work, but it can't keep up with the power drain.
From “Ineffective Supplementation” to “Precision Delivery” – Solving the Placental Transport Dilemma
1. Switching the Transport Hub to a High-Speed Channel
5-methyltetrahydrofolate (the core component of "Magnafolate") is like a custom "maglev train" for the placenta:
· Direct Conversion-Free Delivery: It bypasses the conversion steps via dihydrofolate reductase and 5,10-methylenetetrahydrofolate reductase, directly reaching FR-α in its active form to compensate for the deficiency in transport protein numbers.
· 300% Increased Affinity: Its binding force with FR-α is significantly higher than that of traditional synthetic folic acid. It's like using a powerful magnet to attract transport proteins and forcibly clear blocked channels.
· Enhanced Transplacental Efficiency: Clinical data shows that active folate can increase placental folate transport in obese pregnant women by 47%, injecting a strong stimulant into the "striking" transport hub.
2. Three-Tier Defense for Overweight Moms
· Preconception BMI Screening: Women with a BMI≥28 should increase their daily folic acid intake to 800μg and prioritize active folate.
· Early Pregnancy Placental Monitoring: During prenatal visits at 6-12 weeks of gestation, request an ultrasound to assess chorionic villus development and test serum homocysteine levels (reference value≤15μmol/L). Adjust the supplementation plan dynamically.
· Metabolic Regulation Support: Improve insulin resistance with dietary fiber and probiotics (e.g., consume 25-30g of dietary fiber daily and choose yogurt and other probiotic-rich foods) to create a favorable internal environment for placental transport.
When Jessica switched to a supplement containing 6S-5-methyltetrahydrofolate (Magnafolate), a 16-week recheck revealed that the fetus's neural tube development indicators had returned to normal.

This case unveils a neglected truth:
For overweight pregnant women, the key to folic acid supplementation isn't the "quantity" but the "efficacy" – only by breaking through the placental transport bottleneck can every microgram of folic acid precisely reach the "battlefield" of fetal development.
Risk Alert: Neural tube closure happens between 21-28 days of gestation (equivalent to 35-42 days after the last menstrual period – when most mothers may have just discovered their pregnancy, yet already missed the golden protective period for fetal neural tube development). It is recommended that women with a BMI≥28 start supplementing with active folate three months before conception, under medical guidance, to seize the "golden 72 hours" of fetal development.
Folic Acid Supplementation Q&A for Overweight Pregnant Women
Q: Is eating more folate-rich foods like spinach effective?
A: Natural folate in foods (such as spinach, animal livers) is "naturalized folate." However, folate content in foods is low and unstable. For example, spinach loses 50%-70% of its folate during cooking, and one would need to consume 1.5kg of raw spinach daily to meet the folate requirements during pregnancy. This is impractical. Therefore, supplementation with active folic acid should be the primary approach, with food as a secondary source.
Q: How can I tell if my placental transport efficiency is low?
A: If in early pregnancy, "normal serum folate but elevated homocysteine" or "ultrasound suggests delayed chorionic villus development," or if folate metabolic capacity testing shows a type or CT type and you are overweight, be alert to potential transport efficiency issues and consult a doctor promptly.
Q: What does the MTHFR gene TT type imply?
A: This genotype may reduce folate metabolic enzyme activity by over 70%. Even with normal placental transport, the fetus may still face a risk of folate deficiency, necessitating heightened attention to active folic acid supplementation.
Three-Step Self-Checklist for Folic Acid Supplementation During Pregnancy:
1. Calculate your BMI (≥28 requires caution).
2. Test for the MTHFR gene before conception.
3. At 6 weeks of gestation, proactively request a "chorionic villus ultrasound + homocysteine" combined test.
If any of the following occurs, consult an obstetrician or nutritionist within 48 hours:
· Early pregnancy homocysteine>15μmol/L.
· Ultrasound indicates chorionic villus blood flow resistance index (RI)>0.8.
· MTHFR gene testing shows a TT type with overweight status.
Reference:Hess R J, Rosario F J, Chen Y Y, et al. Decreased placental folate transporter expression and activity in first and second trimester in obese mothers[J]. The Journal of Nutritional Biochemistry, 2020, 77: 108305. DOI: 10.1016/j.jnutbio.2019.108305

 Español
Español Português
Português  русский
русский  Français
Français  日本語
日本語  Deutsch
Deutsch  tiếng Việt
tiếng Việt  Italiano
Italiano  Nederlands
Nederlands  ภาษาไทย
ภาษาไทย  Polski
Polski  한국어
한국어  Svenska
Svenska  magyar
magyar  Malay
Malay  বাংলা ভাষার
বাংলা ভাষার  Dansk
Dansk  Suomi
Suomi  हिन्दी
हिन्दी  Pilipino
Pilipino  Türkçe
Türkçe  Gaeilge
Gaeilge  العربية
العربية  Indonesia
Indonesia  Norsk
Norsk  تمل
تمل  český
český  ελληνικά
ελληνικά  український
український  Javanese
Javanese  فارسی
فارسی  தமிழ்
தமிழ்  తెలుగు
తెలుగు  नेपाली
नेपाली  Burmese
Burmese  български
български  ລາວ
ລາວ  Latine
Latine  Қазақша
Қазақша  Euskal
Euskal  Azərbaycan
Azərbaycan  Slovenský jazyk
Slovenský jazyk  Македонски
Македонски  Lietuvos
Lietuvos  Eesti Keel
Eesti Keel  Română
Română  Slovenski
Slovenski  मराठी
मराठी  Srpski језик
Srpski језик 








 Online Service
Online Service