In the wondrous journey of growing a new life, every
expectant mother is full of hope.
But at the 12-week mark, a single lab sheet flicked on a red light:
homocysteine (Hcy) had become the “invisible killer” lurking in Mom’s and
Baby’s bloodstream.
Today, follow Emily’s experience in the golden window of weeks 11–13 to
decode this danger signal and learn how to defuse it—fast.
The “Verdict” in the Clinic
“Emily.”
The electronic voice, cold as
a scalpel, sliced the silence in the waiting room.
Emily clutched the thin lab
report; her knuckles whitened, the paper’s edge curled from the sweat in her
palm. Each step toward the door felt like walking on cotton.
Inside, Dr. Sarah Collins—nicknamed “the closer” for high-risk
pregnancies—adjusted her gold-rimmed glasses and zeroed in on the scarlet
circle on the page:
“Homocysteine, 8.6 μmol/L.”
Her finger tapped the
number—tap, tap—each rap a hammer blow to Emily’s heart.
“Week twelve, this level is
high.”
“High.” In prenatal visits, that word is the
sword of Damocles.
“Dr. Collins… what will happen?” Emily’s voice quivered, pleading.
“Plainly, it’s an independent
risk factor for preeclampsia.”
“Preeclampsia!” The word
detonated. In her moms’ group chat, the mother who lost her baby at 32 weeks
was still screaming: “My baby is gone, and I almost died on the table!”
Fear seized her throat; black
spots swam before her eyes.
“My baby… will he…?”
“Doctor! My child will be
okay, right? Please…” Tears overflowed.

Dr. Collins handed over a tissue without drama. “Crying won’t solve it.
Emotional swings will only raise your blood pressure—and the risk.”
Ice water on hysteria. Emily
wiped her face, steadied her voice. “Then what do I do?”
For the first time, the
doctor’s gaze held a flicker of approval. She uncapped her pen.
“What folate have you taken
since pre-conception?”
Emily fumbled out a small
white bottle. One glance, and Dr. Collins flicked it back. “Folic acid.”
“Do you know your body’s MTHFR
metabolic capacity? Ninety percent of pregnant women in China don’t.”
Scratch-scratch went the pen.
“Ordinary folic acid is a locked safe; your body is poor at cracking the code,
so the metabolic waste—homocysteine—keeps piling up.”
Emily’s heart sank, but she
seized the keyword. “Is there an unlocked safe?”
“Yes.” Dr. Collins finally met
her eyes. “Naturalization folate—6S-5-methyltetrahydrofolate. No metabolism
required, direct absorption, immediate blood cleanup.”
“Doctor! I’ll buy it right
now!” She half-rose.
“Sit.” The word was soft but
iron. “It’s not enough alone.”
She spun the chart toward
Emily. “Starting today: one hard-boiled egg daily, 100 g lean meat or fish.
Vitamin B12 and B6 are the cleanup crew; they double the efficiency. At your
next visit I want Hcy under seven.”
“Got it!” Emily nodded,
engraving every word.
In the corridor, sunlight stung her eyes. She inhaled, dialed her husband:
“Honey, go to the pharmacy and ask for Magnafolate—ingredient must read
6S-5-methyltetrahydrofolate, letter-perfect.”
“I’m fine. It’s time to
fight.”

She hung up, rested a hand on
her still-flat belly, tears falling again—not from fear, but from the primal
resolve of a mother: “Baby, don’t be afraid. Mom has found the weapon. We’ll
chase the bad guys away together.”
Key Science Box: “Synthetic ” vs. “Active” Folate
This is the pitfall many moms miss:
• Folic acid = synthetic
folate, multi-step liver metabolism required.
• Naturalization folate =
biologically active, ready to use, bypasses MTHFR bottlenecks.

First-Trimester Hcy & Pregnancy Risk
Studies show women with high Hcy in early pregnancy face significantly higher odds of severe preeclampsia—marked by skyrocketing blood pressure, proteinuria, and impaired fetal growth.
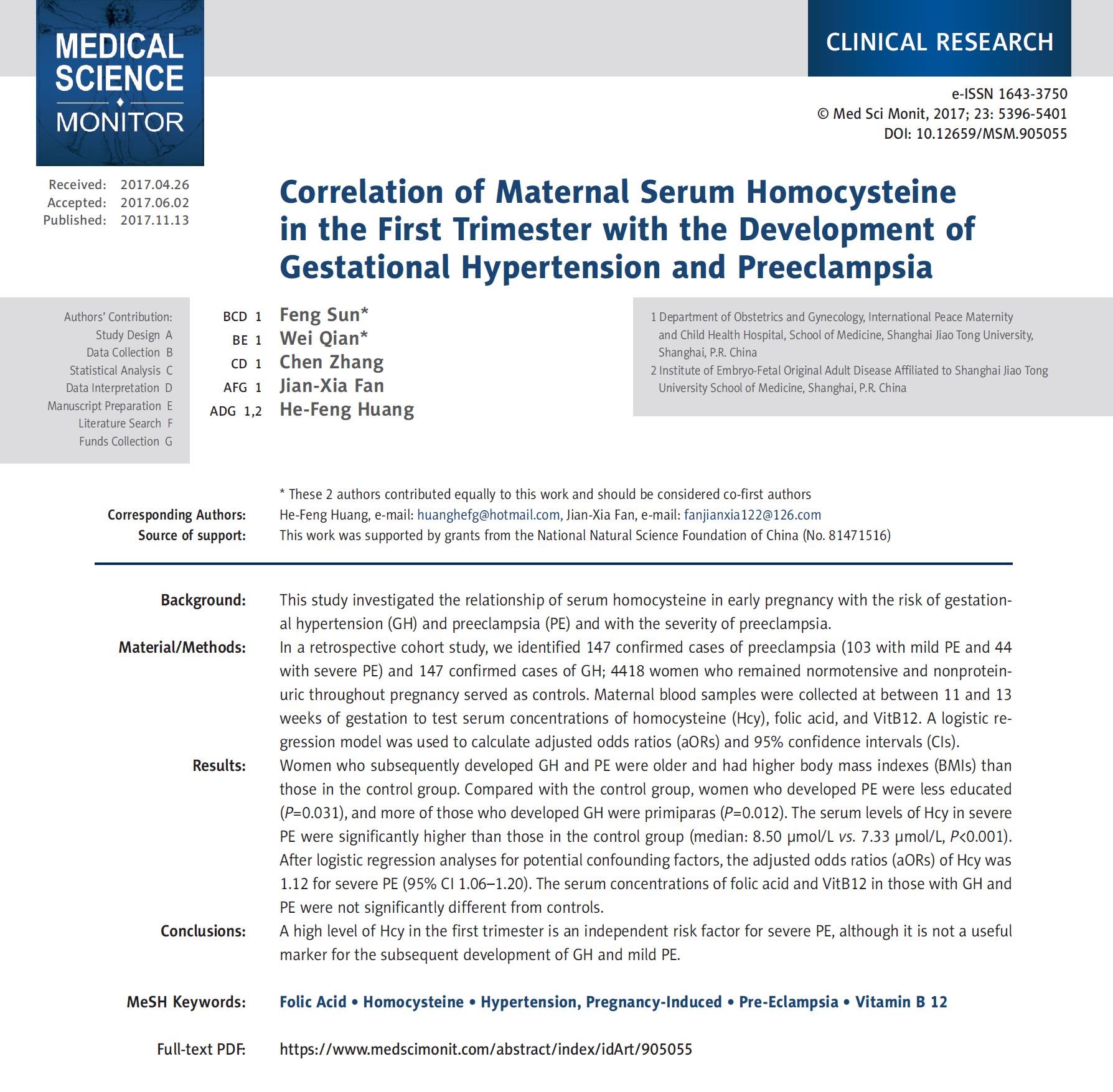
Data from Shanghai Jiao Tong University School of Medicine: median Hcy in severe-preeclampsia mothers was 8.50 μmol/L vs. 7.33 μmol/L in normal pregnancies.
Folate Supplementation Myths
Research also found that moms who kept Hcy in check were the ones whose bodies actually used the active form of folate. Supplementation ≠ utilization—only the utilized form prevents risk.

Build an Extra Shield: Three Simple Rules
Emily switched to Naturalization folate(Magnafolate), added eggs, lean
meats and dairy for B12. At the next visit her Hcy was 6.8 μmol/L.
Dr. Collins smiled: “Give the
body what it can actually use—only then does it work.”
Protect yourself and your baby—just remember these three:
1. At every early-pregnancy visit (weeks 11–13), ask: “What’s my Hcy level?” Early detection means early correction.
2. When choosing folate, look for the word “active.” Active folate (5-methyltetrahydrofolate) requires no second-step metabolism, ideal for women with MTHFR variants or weaker enzymatic capacity—and it sweeps Hcy away efficiently.
3. Recruit the “vascular guardians.” Alongside active folate, vitamin B12 is Hcy’s perfect partner. Daily eggs, lean meats, dairy make the cleanup team stronger.
Epilogue
Now, at every prenatal check, Emily asks for her Hcy number. Sunlight slants across the hospital hallway as she gently cups her rounding belly: “If Mom’s blood carries a little less trouble, you get a little more peace, baby.”

This narrative is adapted from a true case for educational purposes only. Diagnosis and treatment must follow professional medical advice.
References
1. Lian ZL, Liu K, Gu JH, Cheng YZ, et al. Biological characteristics and applications of folate and 5-methyltetrahydrofolate. China Food Additives, 2022(2).
2. Sun F, Qian W, Zhang C, Fan JX, Huang HF. Correlation of maternal serum homocysteine in the first trimester with the development of gestational hypertension and preeclampsia. Med Sci Monit, 2017 Nov 13;23:5396-5401.

 Español
Español Português
Português  русский
русский  Français
Français  日本語
日本語  Deutsch
Deutsch  tiếng Việt
tiếng Việt  Italiano
Italiano  Nederlands
Nederlands  ภาษาไทย
ภาษาไทย  Polski
Polski  한국어
한국어  Svenska
Svenska  magyar
magyar  Malay
Malay  বাংলা ভাষার
বাংলা ভাষার  Dansk
Dansk  Suomi
Suomi  हिन्दी
हिन्दी  Pilipino
Pilipino  Türkçe
Türkçe  Gaeilge
Gaeilge  العربية
العربية  Indonesia
Indonesia  Norsk
Norsk  تمل
تمل  český
český  ελληνικά
ελληνικά  український
український  Javanese
Javanese  فارسی
فارسی  தமிழ்
தமிழ்  తెలుగు
తెలుగు  नेपाली
नेपाली  Burmese
Burmese  български
български  ລາວ
ລາວ  Latine
Latine  Қазақша
Қазақша  Euskal
Euskal  Azərbaycan
Azərbaycan  Slovenský jazyk
Slovenský jazyk  Македонски
Македонски  Lietuvos
Lietuvos  Eesti Keel
Eesti Keel  Română
Română  Slovenski
Slovenski  मराठी
मराठी  Srpski језик
Srpski језик 








 Online Service
Online Service