“It’s one of the most common remarks I hear in the prenatal check-up room: ‘I’d even run ten laps if it means my baby can stay in the womb until 37 weeks!’”

One of the biggest fears after pregnancy is the baby being born prematurely. Especially for early preterm babies born before 32 weeks, they have to overcome multiple challenges such as respiratory issues, infections, and developmental problems, causing constant anxiety for parents.
But did you know?
There is a “low-cost, high-benefit” method that can directly reduce the risk of “spontaneous preterm birth (without medical causes)” by 50%-70%!

This method is supplementing folate 1 year in advance. It is not a trendy miscarriage-prevention formula nor an expensive nutritional supplement. Instead, it is a conclusion validated by data from 34,000 pregnant women across 15 authoritative prenatal centers in the United States (published in the top journal PLOS Medicine with an impact factor of around 12.6). To date, this study has been cited over 400 times, making it highly reliable.
I. What Exactly Does This Study Reveal?
We all know that folate supplementation during pregnancy can prevent neural tube defects. However, this classic cohort study from 2009 uncovered a “hidden benefit” of folate—preventing preterm birth.
Reasons for the Study’s Reliability
- Research Institutions: 15 authoritative prenatal diagnosis centers in the United States, based on a secondary analysis of the “FASTER Trial” (1999-2002). Multi-center data ensures the conclusion is more universally applicable.
- Participants: 34,000 “low-risk singleton pregnant women” (with complete prenatal check-ups, no fetal malformations, or severe underlying diseases). This excludes interference factors, focusing solely on the role of folate.
- Core Question: The relationship between “duration of preconception folate supplementation” and “spontaneous preterm birth (unexplained early labor)”. It only focuses on “natural preterm birth”—the type that requires the most attention.
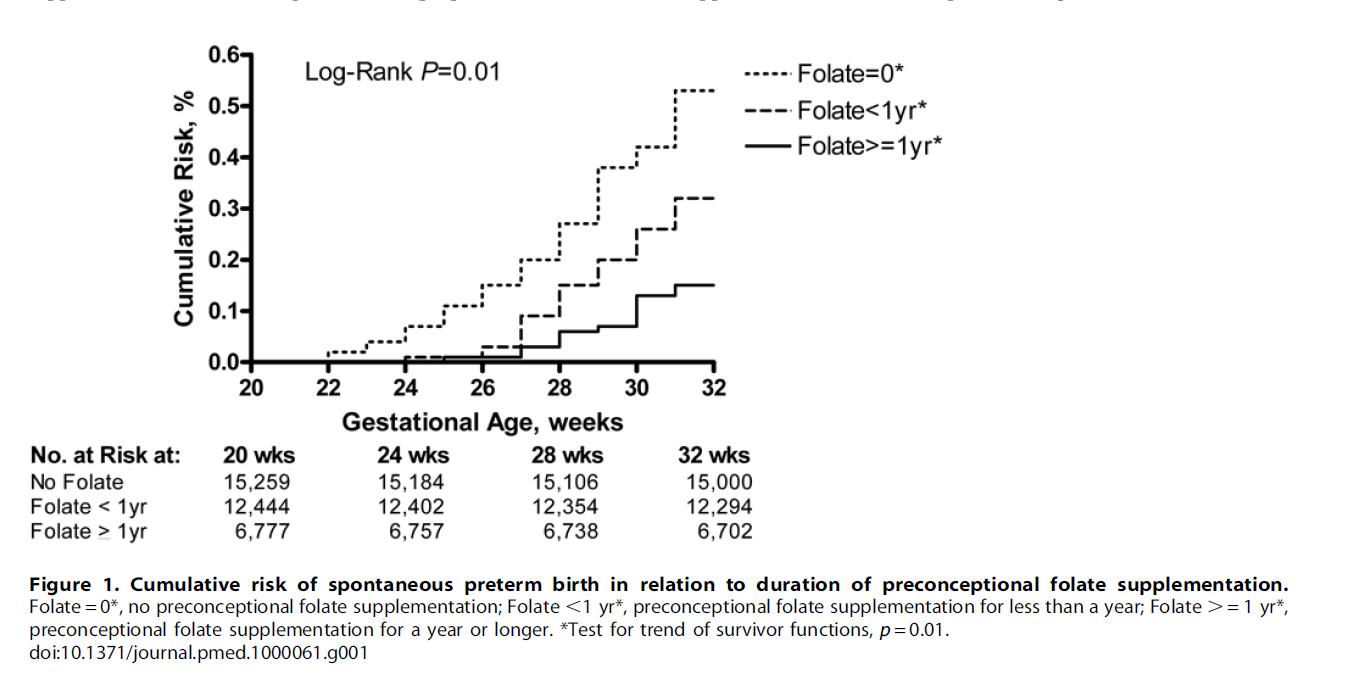
- Grouping Method: Three groups for comparison: ① No supplementation at all; ② Supplemented for less than 1 year; ③ Supplemented for 1 year or more. This directly reflects differences based on “duration of supplementation”.
II. Supplementing Folate for 1 Year Cuts Preterm Birth Risk by Half!
The study used “Hazard Ratio (HR)” to quantify differences. Let’s look at the specific risk reductions:
1. “Extremely Preterm Birth” (20-28 Weeks, the Riskiest Stage)
- No folate supplementation: 2.7 cases per 1,000 women.
- Supplemented for ≥1 year: Only 0.4 cases per 1,000 women. This represents a 70% risk reduction (HR=0.22).
2. “Early Preterm Birth” (28-32 Weeks)
- No folate supplementation: 3.8 cases per 1,000 women.
- Supplemented for ≥1 year: 1.8 cases per 1,000 women. This represents a 50% risk reduction (HR=0.45).
3. “Late Preterm Birth” (After 32 Weeks)
There was almost no difference among the three groups. This indicates that folate only prevents “very early preterm birth” and has no effect on preterm birth close to full term.
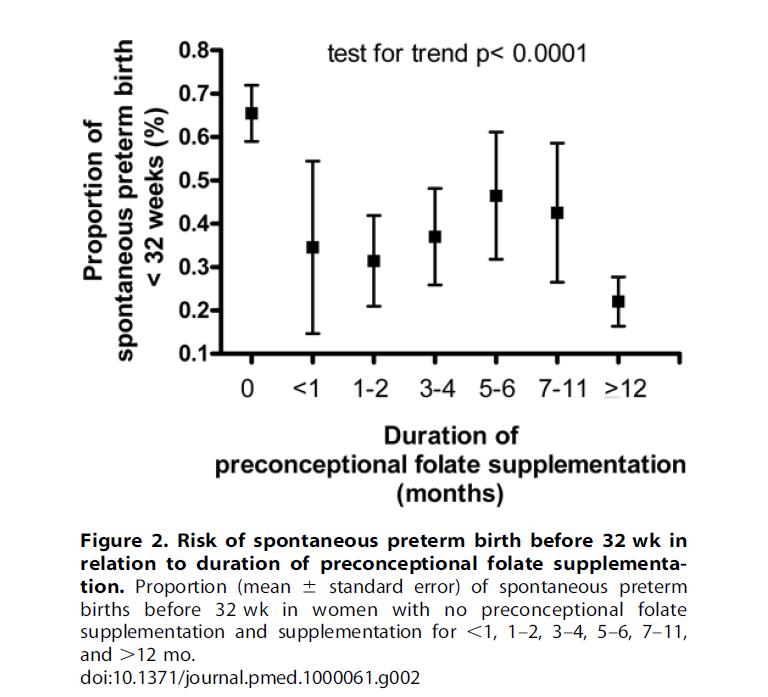
A more critical trend analysis showed: The longer the supplementation duration, the lower the risk. Risk gradually decreases with supplementation periods of 1-2 months, 3-6 months, 7-11 months, and ≥12 months. However, last-minute supplementation (for only 1 month) is basically ineffective!
III. Why Is “6S-5-Methyltetrahydrofolate” Recommended?
The study only states that “folate supplementation is effective”, but the form of folate matters significantly!
Ordinary folic acid (e.g., folic acid tablets) needs to be converted into its active form (5-Methyltetrahydrofolate, abbreviated as 5-MTHF) via “5,10-methylenetetrahydrofolate reductase (MTHFR 677)” before it can be absorbed by the human body.
|
MTHFR Genotype |
Enzyme Activity |
Folate Utilization Capacity |
Risk of Hyperhomocysteinemia |
Proportion in Chinese Population |
|
CC |
100% (Normal) |
High |
Low |
21.6% |
|
CT |
65% (Moderate) |
Moderate |
Moderate |
48.6% |
|
TT |
35% (Low) |
Poor |
High |
29.8% |
 Approximately 78.4% of people in China have
MTHFR gene metabolism disorders, among which about 25% are of the TT genotype
(severe metabolic disorder), making them unable to convert ordinary folic acid
into the usable form at all!
Approximately 78.4% of people in China have
MTHFR gene metabolism disorders, among which about 25% are of the TT genotype
(severe metabolic disorder), making them unable to convert ordinary folic acid
into the usable form at all!
Therefore, “active folate that can be directly absorbed”—6S-5-Methyltetrahydrofolate—is a better choice for us. In particular, “Naturalization folate (Magnafolate)”, whose safety has been tested by the Shanghai CDC to be at the “practically non-toxic level”, is more suitable for meeting maternal and infant safety needs. No toxic or harmful raw materials such as formaldehyde, p-toluenesulfonate, or heavy metals are used in its production process. Its harmful impurity JK12A is less than 0.1%, only one-tenth of that in overseas competing products.
Recommendations for Folate Supplementation
|
Stage |
Daily Dosage |
Folate Form |
Key Notes |
|
Preconception (≥12 months in advance) |
400-800μg |
5-MTHF (Active) |
Lay the foundation! Ensure the body’s folate reserves are “sufficient”. |
|
First Trimester (Weeks 1-12) |
400-800μg |
5-MTHF (Active) |
Dual protection: Prevent neural tube defects (critical period for fetal brain/spinal cord development) + continue to reduce preterm birth risk. |
|
Second & Third Trimesters (Weeks 13 to Delivery) |
400μg |
5-MTHF (Active) |
Focus on preventing “infection-related preterm birth”: Folate has anti-inflammatory effects and reduces unexplained preterm birth. Dosage can be reduced, but do not stop supplementation! |
IV. Avoid Pitfalls! Don’t Fall for These 3 Misconceptions
Based on the study and clinical practice, avoid these mistakes:
- “Taking folate means no risk of preterm birth”? Incorrect!
Folate only prevents “spontaneous preterm birth”. It is ineffective for “indicated preterm birth” caused by preeclampsia, placental abruption, or fetal malformations. Regular prenatal check-ups, controlling blood pressure and blood sugar, and preventing infections are more important.
- “I’m in good health, so I don’t need to supplement for 1 year”?
Regardless of age, BMI, or smoking status (all risk factors for preterm birth), supplementing for “≥1 year” provides protective effects. Even “low-risk mothers” can gain an extra layer of protection by starting supplementation in advance.
- “Taking folate means I don’t need to care about other factors”?
Folate is an “auxiliary protective measure”, not a “universal insurance”! Quitting smoking, limiting alcohol intake, avoiding staying up late, and minimizing exposure to harmful substances—these healthy habits are the “foundation” for preventing preterm birth.
V. Preconception Tips
- Don’t wait until “confirmation of pregnancy” to start supplementation—folate needs to be “stocked up in advance”! Many people don’t notice they are pregnant in the first 3 months, so by the time pregnancy is confirmed, they have already missed the critical period for folate reserve.
-
Don’t choose folate based solely on low price—folic acid is not
significantly effective for 78.4% of Chinese people. Directly choose
“6S-5-Methyltetrahydrofolate”; just check the ingredient list (look for
this term).

Starting today, add “supplementing active folate 1 year in advance” to your preconception checklist. It costs only a few cents per day, but gives your baby more time to “mature” in the womb!
References
[1] Bukowski R, et al. Preconceptional folate supplementation and the risk of spontaneous preterm birth: a cohort study. PLOS Med. 2009 May;6(5):e1000061.
[2] Lian Z L, et al. Biological Characteristics and Applications of Folate and 5-Methyltetrahydrofolate. China Food Additives, 2022, No.2.

 Español
Español Português
Português  русский
русский  Français
Français  日本語
日本語  Deutsch
Deutsch  tiếng Việt
tiếng Việt  Italiano
Italiano  Nederlands
Nederlands  ภาษาไทย
ภาษาไทย  Polski
Polski  한국어
한국어  Svenska
Svenska  magyar
magyar  Malay
Malay  বাংলা ভাষার
বাংলা ভাষার  Dansk
Dansk  Suomi
Suomi  हिन्दी
हिन्दी  Pilipino
Pilipino  Türkçe
Türkçe  Gaeilge
Gaeilge  العربية
العربية  Indonesia
Indonesia  Norsk
Norsk  تمل
تمل  český
český  ελληνικά
ελληνικά  український
український  Javanese
Javanese  فارسی
فارسی  தமிழ்
தமிழ்  తెలుగు
తెలుగు  नेपाली
नेपाली  Burmese
Burmese  български
български  ລາວ
ລາວ  Latine
Latine  Қазақша
Қазақша  Euskal
Euskal  Azərbaycan
Azərbaycan  Slovenský jazyk
Slovenský jazyk  Македонски
Македонски  Lietuvos
Lietuvos  Eesti Keel
Eesti Keel  Română
Română  Slovenski
Slovenski  मराठी
मराठी  Srpski језик
Srpski језик 








 Online Service
Online Service