A 28-week pregnant woman anxiously asked during a clinic visit: "Doctor, I've been feeling fatigued lately, and tests show my folate levels are low. Could this lead to an early delivery?"

Preterm birth (defined as delivery between 28 and less than 37 weeks of gestation) is one of the most common perinatal complications, with a global incidence of approximately 11%. It not only threatens neonatal survival but may also lead to long-term health issues. In obstetric clinics, we frequently encounter expectant mothers with similar concerns. Many are aware that folate is an "essential nutrient during pregnancy," but their understanding often stops at "preventing fetal neural tube defects." What you might not know is that folate's role extends far beyond this.
Key Research Findings
A landmark study published in the American Journal of Obstetrics and Gynecology (AJOG) in 2004 provided a clear answer: Insufficient folate levels during the second trimester can increase the risk of preterm birth by nearly 80%.
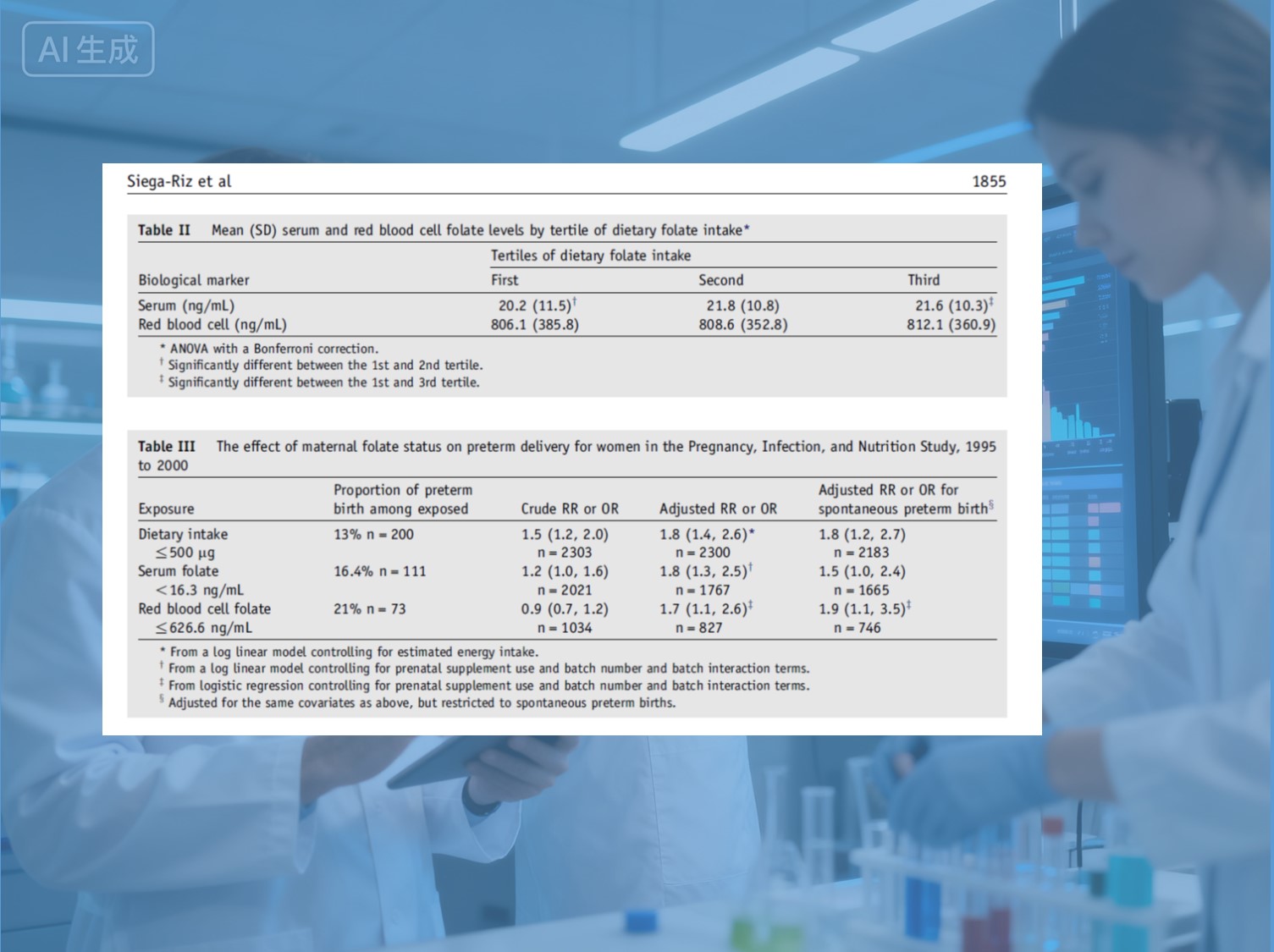
This prospective study, led by the University of North Carolina, followed 2,468 pregnant women and found that those with a daily folate intake of ≤500 μg during the second trimester had an 80% increased risk of preterm birth (RR=1.8). Notably, this risk existed independently of other factors—even after adjusting for over 10 potential confounding variables such as age, ethnicity, smoking status, and economic level, the association remained significant.
01 Why Are Second-Trimester Folate Levels So Critical?
Previously, the importance of folate supplementation was primarily linked to preventing neural tube defects in the first trimester. This AJOG study highlights a crucial shift: the second trimester (24–29 weeks) is a "golden window" of rapid fetal growth, during which folate nutritional status is equally vital.
During this period, folate serves as a "cornerstone" for DNA synthesis and cell proliferation, directly supporting several core physiological processes:
- Precise Development of the Placental Vascular Network
- Rapid Division and Growth of Fetal Cells
- Significant Expansion of Maternal Blood Volume
If folate supply "drops off," it may lead to restricted placental development, reduced uterine blood flow perfusion, and subsequently trigger the body's preterm birth warning mechanism.
Study data provides strong evidence:
- Serum folate < 16.3 ng/mL → Preterm birth risk increased by 80%
- Red blood cell folate ≤ 626.6 ng/mL → Preterm birth risk increased by 70%
The conclusion is clear and consistent: Folate insufficiency in the second trimester is an independent risk factor for preterm birth.
02 Common Misconceptions About Folate Supplementation: "Taking" Does Not Equal "Absorbing"
In clinical practice, many pregnant women who consistently supplement with folate still face a risk of preterm birth. The issue may lie in absorption efficiency.
Conventional synthetic folic acid requires complex metabolic conversion:
it must first be converted to dihydrofolate by dihydrofolate reductase in the
liver, then to tetrahydrofolate, and finally catalyzed by the MTHFR enzyme to
produce 6S-5-methyltetrahydrofolate (active folate) before the body can utilize
it.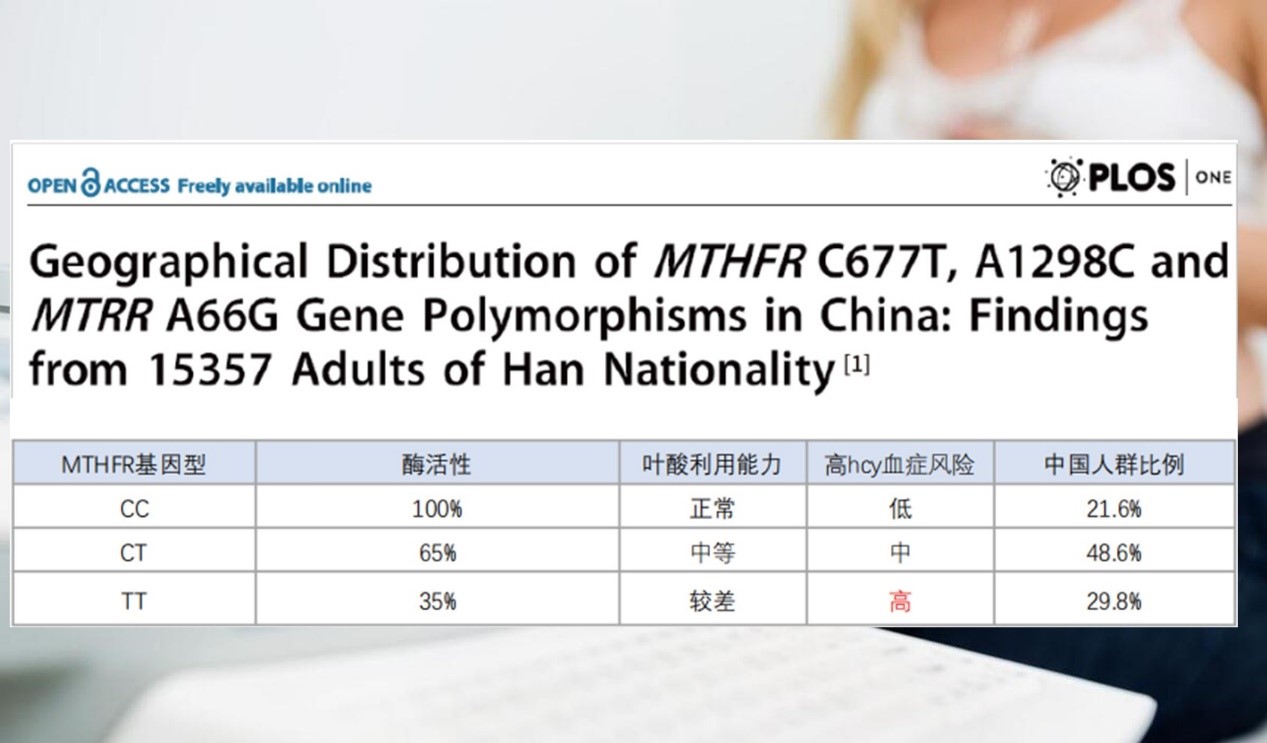
However, approximately 78.4% of the Chinese population carries MTHFR gene mutations, leading to significantly reduced enzyme activity. This means that even with adequate supplementation of synthetic folic acid, conversion impairments may prevent it from functioning effectively.

This is where the value of Magnafolate (6S-5-methyltetrahydrofolate) lies. As an active folate that requires no metabolic conversion, Magnafolate can directly enter the bloodstream, rapidly increasing serum and red blood cell folate levels, effectively bypassing absorption barriers caused by genetic mutations.
03 Scientific Folate Supplementation: Three Recommendations for Expectant Mothers
Based on AJOG research evidence and clinical practice, we recommend:

- Supplement Throughout Pregnancy: Folate is needed not only in the first trimester but must be ensured as adequate during the second trimester. Research shows that the association between low folate levels in the second trimester and preterm birth is even stronger than indicators in the first trimester. It is advised to supplement at least until 28 weeks gestation, and ideally continue until delivery if possible.
- Choose Highly Absorbable Active Folate: For women with MTHFR gene mutations or concerns about conversion efficiency, prioritize active folates like Magnafolate. Studies indicate that active folate has approximately 70% higher bioavailability than regular folic acid, more effectively increasing serum folate concentrations and reducing preterm birth risk.
-
Individualize
Dosage: The general
recommendation for pregnant women is a daily supplement of 400–800 μg of
folate. However, for those with a history of preterm birth, multiple
pregnancies, or folate metabolism disorders, the dosage should be
appropriately increased or active folate should be selected under medical
guidance.
04 From Nutrition to Life: Folate's Protection Throughout Pregnancy
The profound significance of this AJOG study is that it redefines the value of folate: it is not only the "safety cornerstone" for preventing birth defects in the first trimester but also a "guardian throughout pregnancy" protecting fetal health until full term.

Therefore, for women planning pregnancy or already in the second trimester, we recommend taking the following three proactive steps:
- Proactive Assessment: Consult a doctor early and undergo folate level testing to understand your nutritional status.
- Precise Selection: Discuss your supplementation plan with your doctor. For those concerned about folate absorption efficiency, learn about the option of active folate (such as Magnafolate). It is a form of folate that can be utilized directly without complex in vivo conversion, potentially helping to address absorption issues in some individuals.
- Consistent Adherence: The protective role of folate spans the entire pregnancy. View folate supplementation as a health commitment lasting from preconception through the third trimester.
Nutritional investment in early life is the health investment with the highest return. Choosing a scientifically reliable supplementation method is not only about avoiding risks but also about laying a solid foundation for a child's lifelong health.
【Reminder】
This content is based on the 2004 AJOG study and subsequent evidence-based medical findings, aiming to popularize knowledge about prenatal nutrition. Individual circumstances vary; please follow your doctor's advice regarding specific supplementation plans.
References:
[1] Siega-Riz AM, et al. Second trimester folate status and preterm birth. Am J Obstet Gynecol. 2004;191:1851-7.
[2] Yang B, Liu Y, Li Y, et al. Geographical Distribution of MTHFR C677T, A1298C and MTRR A66G Gene Polymorphisms in China: Findings from 15357 Adults of Han Nationality. PLOS ONE, 2013, 8(3): e57917. doi:10.1371/journal.pone.0057917.
[3] Lian Zenglin, Liu Kang, Gu Jinhua, Cheng Yongzhi, et al. Biological Characteristics and Applications of Folic Acid and 5-Methyltetrahydrofolate. China Food Additives, 2022, Issue 2.

 Español
Español Português
Português  русский
русский  Français
Français  日本語
日本語  Deutsch
Deutsch  tiếng Việt
tiếng Việt  Italiano
Italiano  Nederlands
Nederlands  ภาษาไทย
ภาษาไทย  Polski
Polski  한국어
한국어  Svenska
Svenska  magyar
magyar  Malay
Malay  বাংলা ভাষার
বাংলা ভাষার  Dansk
Dansk  Suomi
Suomi  हिन्दी
हिन्दी  Pilipino
Pilipino  Türkçe
Türkçe  Gaeilge
Gaeilge  العربية
العربية  Indonesia
Indonesia  Norsk
Norsk  تمل
تمل  český
český  ελληνικά
ελληνικά  український
український  Javanese
Javanese  فارسی
فارسی  தமிழ்
தமிழ்  తెలుగు
తెలుగు  नेपाली
नेपाली  Burmese
Burmese  български
български  ລາວ
ລາວ  Latine
Latine  Қазақша
Қазақша  Euskal
Euskal  Azərbaycan
Azərbaycan  Slovenský jazyk
Slovenský jazyk  Македонски
Македонски  Lietuvos
Lietuvos  Eesti Keel
Eesti Keel  Română
Română  Slovenski
Slovenski  मराठी
मराठी  Srpski језик
Srpski језик 








 Online Service
Online Service