A common question in preconception counseling is: "I take folic acid daily as prescribed, and my blood tests show 'normal' levels—so why do I keep experiencing pregnancy loss?"
This question points to a critical yet often overlooked issue: the problem is not inadequate intake, but impaired folate metabolism.
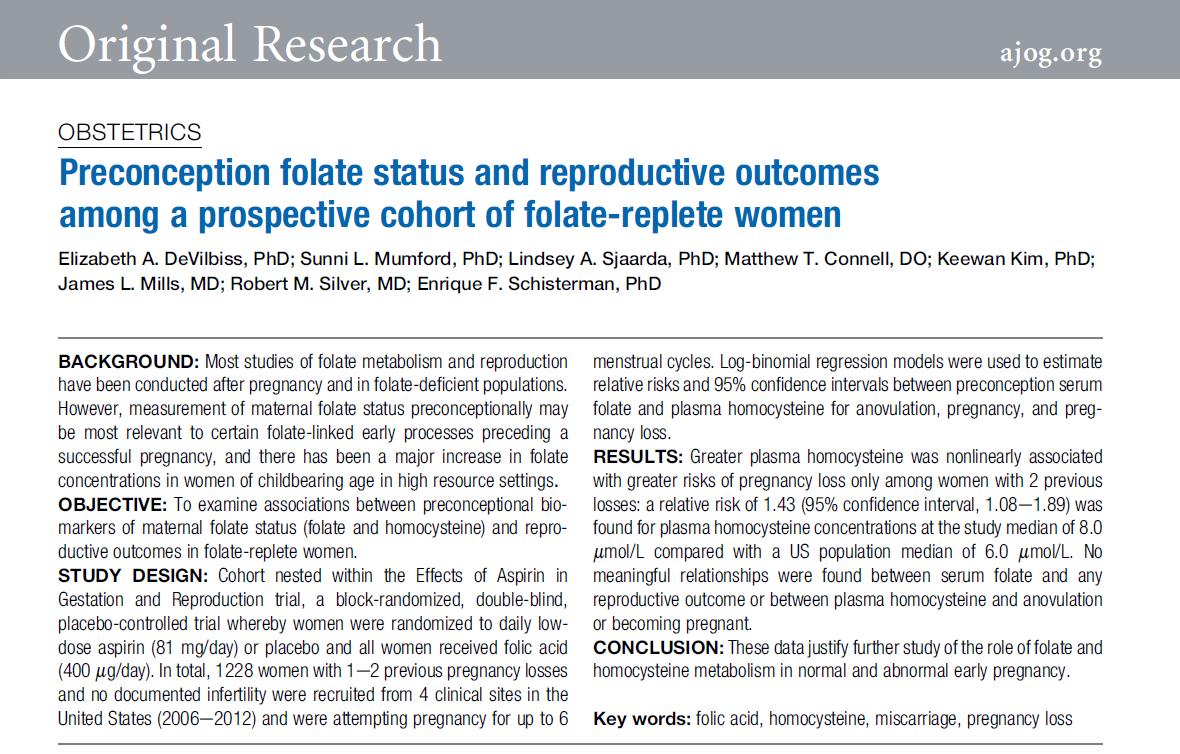
A 2019 study published in the American Journal of Obstetrics & Gynecology (a leading journal in obstetrics with an impact factor of 9.8) addressed this precise concern.
I. The Key Factor Is Metabolic Efficiency, Not Supplemental Dosage
Researchers prospectively followed 1,228 women with a history of one or two prior miscarriages who were consistently supplementing with 400 µg of folic acid daily. The findings revealed:
· No statistically significant association between serum folate concentration and subsequent miscarriage risk.
· A clear dose-dependent relationship with homocysteine (Hcy): among women with two prior losses, each 2 µmol/L increase in Hcy (e.g., from 6 µmol/L to 8 µmol/L) was associated with a 43% increase in miscarriage risk.
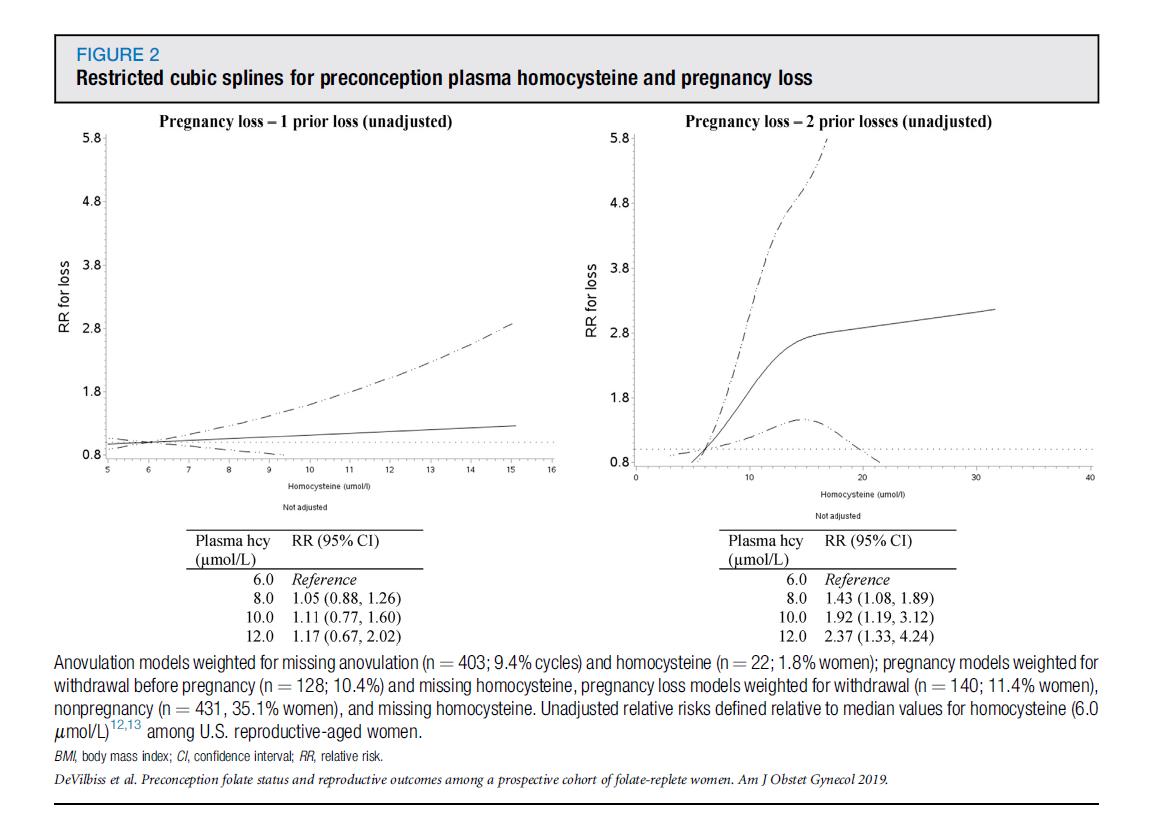
These results demonstrate that with adequate folic acid intake, pregnancy outcomes depend on folate metabolic capacity, not serum levels alone.
Folic acid must be converted to its biologically active form, 6S-5-methyltetrahydrofolate (5-MTHF), to serve as a methyl donor in the remethylation pathway that clears homocysteine. This conversion requires key enzymes including dihydrofolate reductase (DHFR) and 5,10-methylenetetrahydrofolate reductase (MTHFR).
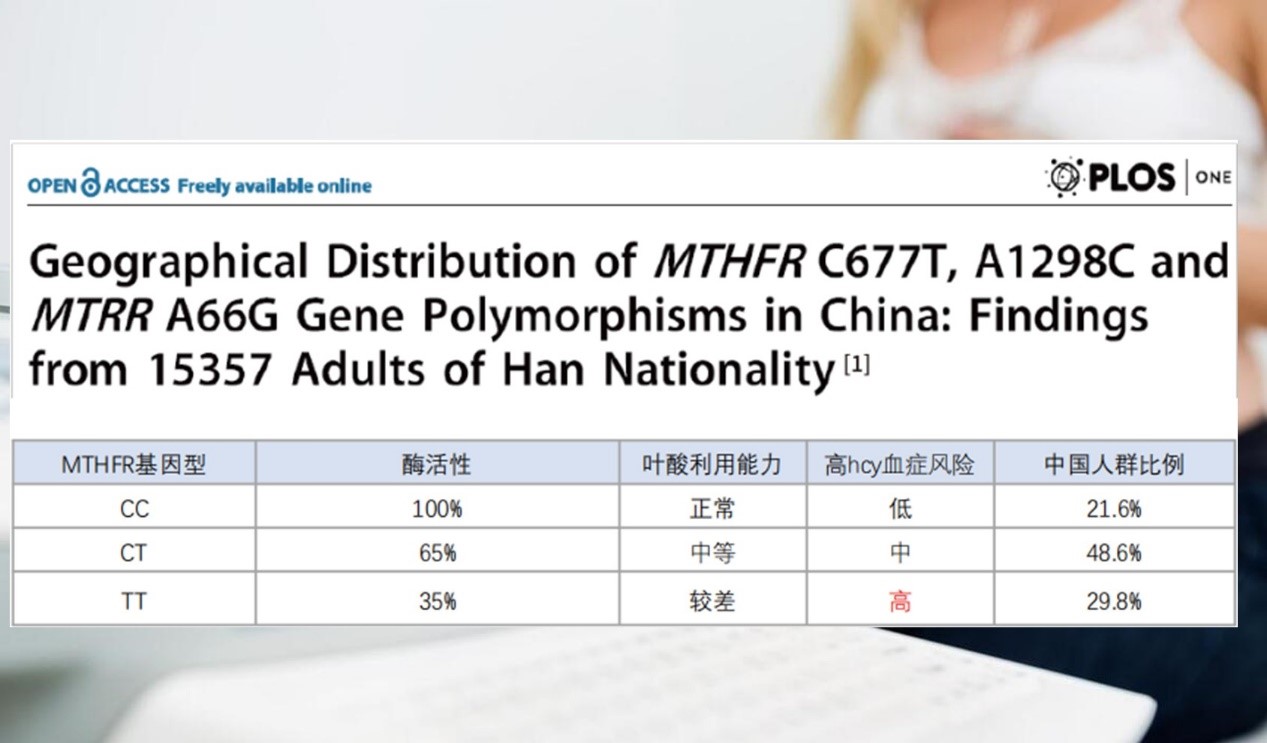
II. The Underlying Cause: Common Genetic Polymorphisms in MTHFR
Population studies in China indicate that approximately 78.4% of individuals carry MTHFR gene polymorphisms (such as C677T and A1298C variants), which reduce enzyme activity to 30–70% of normal function.
This metabolic bottleneck impairs the generation of usable 5-MTHF, leading to inefficient homocysteine clearance and accumulation of hyperhomocysteinemia (HHcy)—a metabolically harmful state.
For women attempting conception, elevated Hcy levels can:
· Disrupt embryo implantation by impairing trophoblast vascularization and uteroplacental perfusion
· Exacerbate oxidative stress, compromising the early embryonic microenvironment
· Promote a prothrombotic state, hindering uterine spiral artery remodeling and compromising placental function
III. Clinical Approach: Screen Hcy and Optimize With Active 5-MTHF
For patients with recurrent pregnancy loss or Hcy levels ≥8 µmol/L, standard folic acid supplementation is often insufficient to overcome metabolic inefficiencies and lower Hcy effectively.
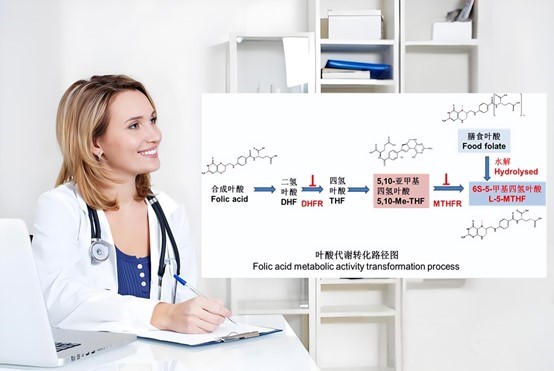
In such cases, direct supplementation with active folate (6S-5-MTHF)—which bypasses MTHFR-dependent conversion—has been shown to reduce Hcy levels efficiently. Products with established safety profiles (e.g., Magnafolate) provide bioavailable 5-MTHF directly into the methionine cycle.

Evidence-Based Recommendations:
1. Preconception Screening: Measure both serum Hcy and folate levels to identify metabolic bottlenecks.
2. Personalized Supplementation: For those with metabolic impairment or HHcy, replace standard folic acid with active 5-MTHF.
3. Adjunctive Support: Co-administer vitamins B12 and B6 under medical supervision to optimize one-carbon metabolism.
4. Professional Oversight: All supplementation strategies require physician guidance to prevent potential adverse effects from unsupervised high-dose regimens.
References
1. Mumford SL, et al. Preconception folate status and reproductive outcomes among a prospective cohort of folate-replete women. Am J Obstet Gynecol. 2019;220(4):399.e1-399.e10.
2. Yang B, et al. Geographical Distribution of MTHFR Gene Polymorphisms in China. PLoS One. 2013;8(3):e57917.
3. Biological Characteristics and Applications of Folate and 5-Methyltetrahydrofolate. China Food Additives. 2022(2).

 Español
Español Português
Português  русский
русский  Français
Français  日本語
日本語  Deutsch
Deutsch  tiếng Việt
tiếng Việt  Italiano
Italiano  Nederlands
Nederlands  ภาษาไทย
ภาษาไทย  Polski
Polski  한국어
한국어  Svenska
Svenska  magyar
magyar  Malay
Malay  বাংলা ভাষার
বাংলা ভাষার  Dansk
Dansk  Suomi
Suomi  हिन्दी
हिन्दी  Pilipino
Pilipino  Türkçe
Türkçe  Gaeilge
Gaeilge  العربية
العربية  Indonesia
Indonesia  Norsk
Norsk  تمل
تمل  český
český  ελληνικά
ελληνικά  український
український  Javanese
Javanese  فارسی
فارسی  தமிழ்
தமிழ்  తెలుగు
తెలుగు  नेपाली
नेपाली  Burmese
Burmese  български
български  ລາວ
ລາວ  Latine
Latine  Қазақша
Қазақша  Euskal
Euskal  Azərbaycan
Azərbaycan  Slovenský jazyk
Slovenský jazyk  Македонски
Македонски  Lietuvos
Lietuvos  Eesti Keel
Eesti Keel  Română
Română  Slovenski
Slovenski  मराठी
मराठी  Srpski језик
Srpski језик 








 Online Service
Online Service