“Doctor, my best friend took folic acid her entire pregnancy and her baby was still born with a heart defect. Could the same thing happen to me?” Emily, 23 weeks pregnant, blurted out the fear she had carried for days.

Emily’s worry is far from rare.
Many expectant mothers believe that swallowing a folic-acid tablet is the end of the story. They miss one critical plot twist: the folate you swallow is not necessarily the folate your body can use.
Why does risk remain even after supplementation?
Standard folic acid is not biologically active. Before it can do any good it must be converted by the enzyme MTHFR into the body-ready form, 6S-5-methyltetrahydrofolate.
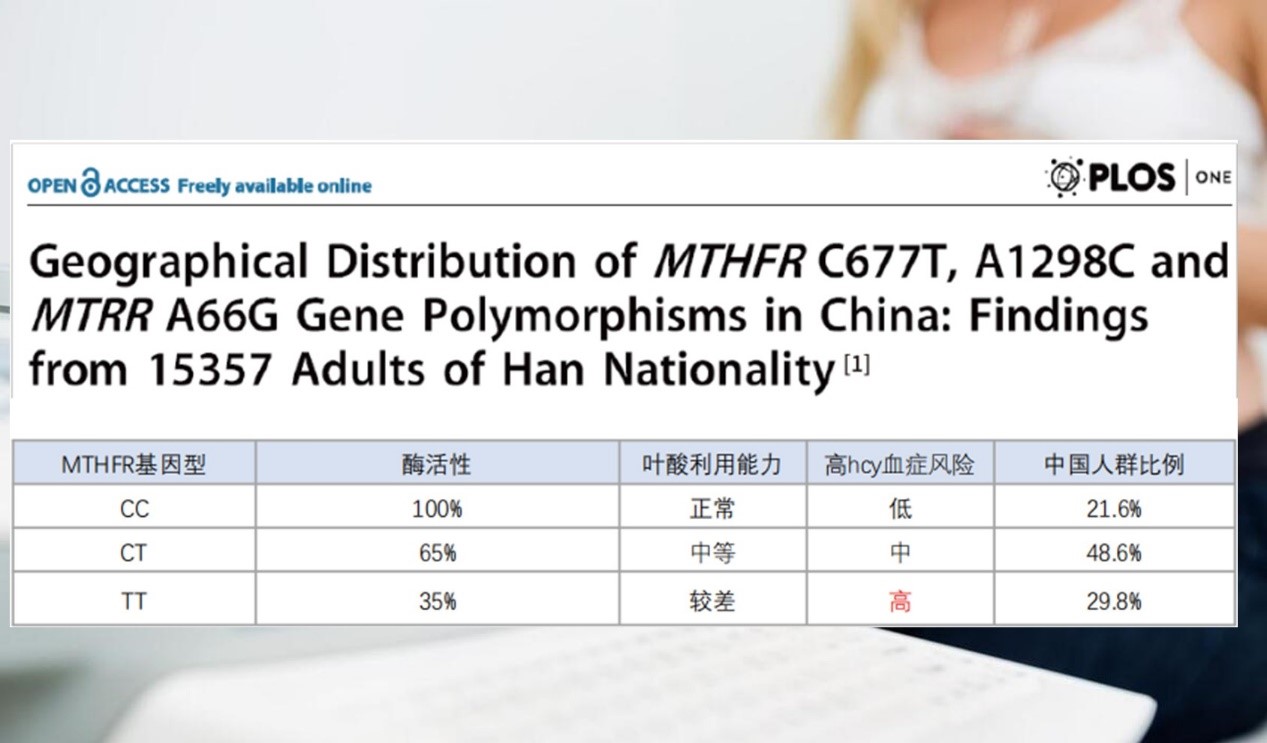
Roughly 78 % of Chinese women carry an MTHFR 677 variant (CT or TT) that slashes enzyme activity to 35–65 %. In these women much of the ingested folic acid never converts; it lingers in the blood as unmetabolized folic acid (UMFA) and may even raise the risk of congenital heart disease.
What the numbers say: gene variant⇄heart-defect risk
In March 2006 the European Heart Journal published a dual-design study (case–control plus family-based) from Radboud University Medical Center.
Among 165 families with congenital heart disease (CHD) and 220 control families, mothers who carried the MTHFR 677 CT or TT genotype and had NOT taken periconceptional folate supplements were far more likely to have a child with conduction-type heart defects (OR 3.3 and 6.3, respectively).
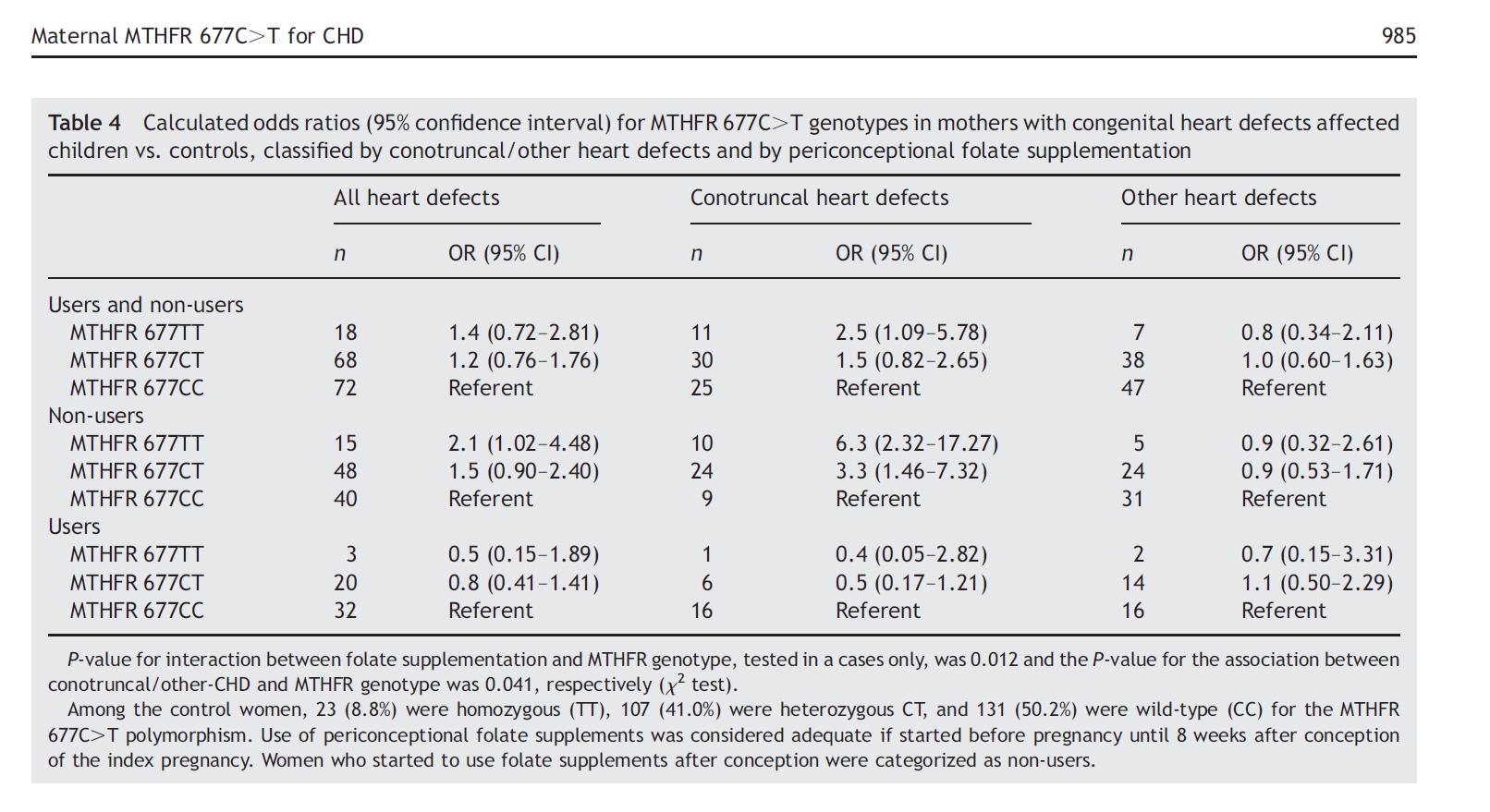
A significant gene–supplement interaction (P = 0.012) underscored the need for genotype-aware supplementation.
Chinese data mirror the finding.
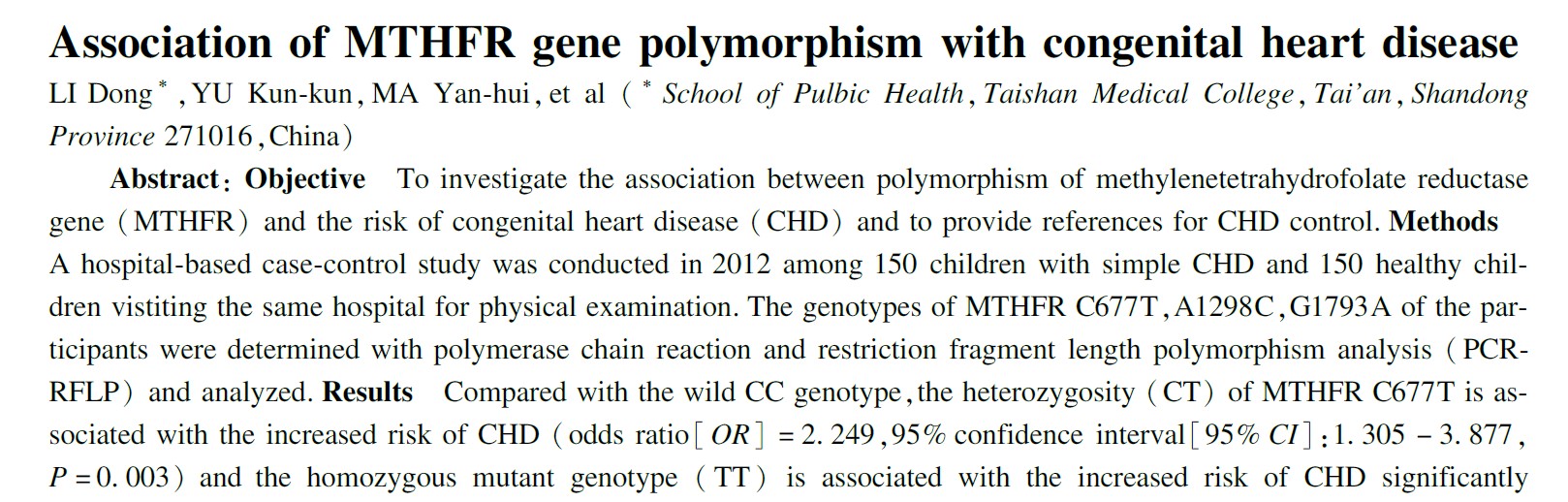
A study from Qilu Children’s Hospital of Shandong University showed that the T allele of MTHFR C677T increases CHD odds 1.8-fold; TT and CT genotypes push the risk to 3.1-fold and 2.2-fold.
The fix: choose the active form
Because the genetic road-block is common, the safest route is to bypass it entirely. Magnafolate—the pure, crystalline form of 6S-5-methyltetrahydrofolate—has been certified “practically non-toxic” by the Shanghai Center for Disease Control and Prevention.

Compared with folic acid it offers three advantages:
Safety: toxicology data show
no observable adverse effects at thousands of times the human dose.
Efficacy: no MTHFR conversion required; serum and
red-cell folate rise quickly, eliminating “I took it but my body ignored it.”
Precision: works regardless of MTHFR 677 genotype,
cutting the risk tied to poor folate metabolism.
Closing thought: let science guard the very first chapter of life
For every woman who is trying to conceive or already pregnant, each nutrition decision is a love letter to the child she has not yet met. Knowing your MTHFR status and choosing the right folate is no longer optional—it is basic prenatal care. With Magnafolate, mothers can override common genetic variation and give their babies the head-start they deserve.

Reminder: This article is for educational purposes only and is not a substitute for personal medical advice. Always consult a qualified health professional before starting any supplement.
Note: The story of “Emily” is a composite sketch based on common clinical scenarios and published research, not an actual patient.
References
1. van der Put NM, Steegers-Theunissen RP, Lindemans J, et al. Maternal MTHFR 677C>T is a risk factor for congenital heart defects: effect modification by periconceptional folate supplementation. Eur Heart J. 2006.
2. Li D, Yu K, Ma Y, et al. Association between MTHFR C677T polymorphism and congenital heart disease in Chinese population. Chin J Public Health. 2016;32(10):1373-1381.
3. Lian Z, Liu K, Gu J, Cheng Y. Biological characteristics and application of folate and 5-methyltetrahydrofolate. China Food Additives. 2022;(2).

 Español
Español Português
Português  русский
русский  Français
Français  日本語
日本語  Deutsch
Deutsch  tiếng Việt
tiếng Việt  Italiano
Italiano  Nederlands
Nederlands  ภาษาไทย
ภาษาไทย  Polski
Polski  한국어
한국어  Svenska
Svenska  magyar
magyar  Malay
Malay  বাংলা ভাষার
বাংলা ভাষার  Dansk
Dansk  Suomi
Suomi  हिन्दी
हिन्दी  Pilipino
Pilipino  Türkçe
Türkçe  Gaeilge
Gaeilge  العربية
العربية  Indonesia
Indonesia  Norsk
Norsk  تمل
تمل  český
český  ελληνικά
ελληνικά  український
український  Javanese
Javanese  فارسی
فارسی  தமிழ்
தமிழ்  తెలుగు
తెలుగు  नेपाली
नेपाली  Burmese
Burmese  български
български  ລາວ
ລາວ  Latine
Latine  Қазақша
Қазақша  Euskal
Euskal  Azərbaycan
Azərbaycan  Slovenský jazyk
Slovenský jazyk  Македонски
Македонски  Lietuvos
Lietuvos  Eesti Keel
Eesti Keel  Română
Română  Slovenski
Slovenski  मराठी
मराठी  Srpski језик
Srpski језик 








 Online Service
Online Service