The Invisible Burden: Insulin Resistance and Metabolic Risks in PCOS
Many women with polycystic ovary syndrome (PCOS) recognize a quiet burden—insulin resistance can throw hormone balance off course and quietly raise the future risk of type 2 diabetes.

- CC has normal enzyme activity
- CT shows reduced activity
- TT exhibits a marked drop in activity
Lower activity means folate cannot be efficiently transformed into a usable form, leaving some circulating in the blood as **Unmetabolized Folic Acid** and gradually accumulating.
---
Risk Signals in the Data: An Egyptian PCOS Study
In early 2019, a study in the *Journal of Gene Medicine* directly linked this genetic difference to health risk.
Researchers enrolled 200 women with PCOS meeting the Rotterdam criteria, half with insulin resistance (IR) and half without.
The groups were matched for age and living conditions, and factors such as medication, alcohol, and tobacco were excluded.Using PCR-RFLP testing, they found that among those with IR, the **TT genotype** accounted for 19%, versus only 6% in the non-IR group—more than triple the rate. Translated into risk, TT carriers had **5.2 times** the odds of developing IR compared to other genotypes. The T allele frequency was 45.5% in the IR group and 30% in the non-IR group; all genetic models pointed to the same conclusion.
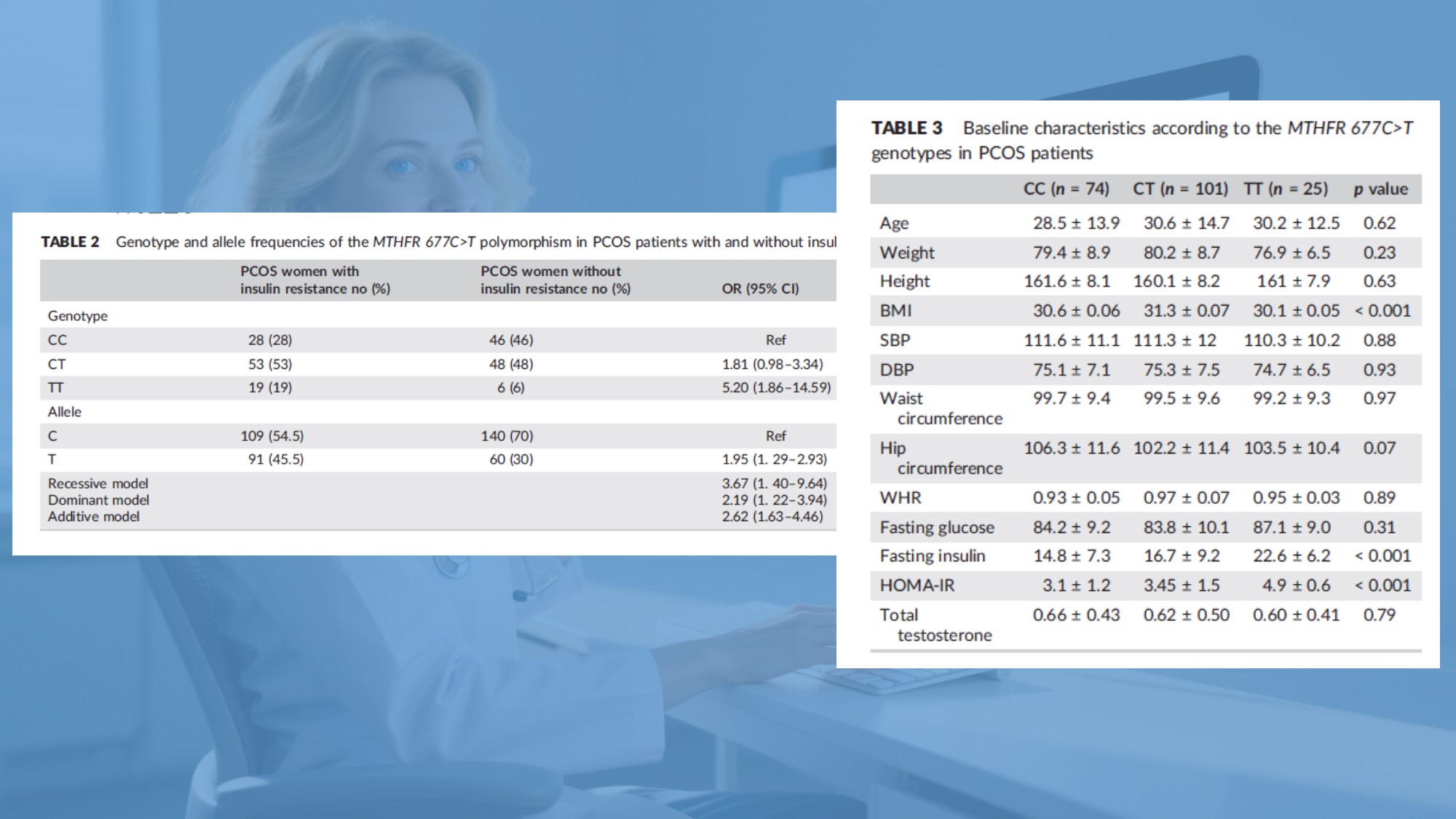
The authors clearly stated that, in Egyptian women with PCOS, the *MTHFR* 677C>T polymorphism is an independent biomarker for insulin resistance. Reduced enzyme activity leads to elevated homocysteine, nudging metabolism toward an unfavorable path.
The team recommended including *MTHFR* genetic testing in early metabolic risk assessment for PCOS, suggesting that early intervention in folate metabolism abnormalities might help prevent diabetes.This reveals a commonly overlooked blind spot: individuals differ in their ability to metabolize folate. Some, due to low enzyme activity, cannot convert it effectively; folate merely circulates in the blood without being used. For women with PCOS who are **TT** or **CT** genotype, using traditional synthetic **folic acid** may yield poor results—failing to raise usable folate levels and possibly adding metabolic strain.---
Bypassing the Traffic Jam: The Advantage of Active Folate
When the road is blocked, why not deliver the finished product straight away?

Practical Advice: Making Supplementation Fit You
You might ask, what should I actually do?
- If possible, consider MTHFR genetic testing to clarify your genotype and guide a personalized plan.
- For women with PCOS, especially those at higher IR risk, choosing an active folate from the start saves effort and avoids the variable effectiveness caused by genetic differences.
- For those preparing for pregnancy, with elevated homocysteine, or other special health considerations, consult a physician or dietitian for individualized dosing.
Managing insulin resistance and metabolic health in PCOS is a long-term endeavor; patience matters.

References
- [Study Author Team]. Genetic polymorphism of methylenetetrahydrofolate reductase is associated with insulin resistance in Egyptian women with polycystic ovary syndrome. *Journal of Gene Medicine*, 2019, 21(1): e3039.
- Lian Zenglin, Liu Kang, Gu Jinhua, Cheng Yongzhi. Biological characteristics and applications of folate and 5-Methyltetrahydropteroic acid. *China Food Additives*, 2022(2): 229–238.

 Español
Español Português
Português  русский
русский  Français
Français  日本語
日本語  Deutsch
Deutsch  tiếng Việt
tiếng Việt  Italiano
Italiano  Nederlands
Nederlands  ภาษาไทย
ภาษาไทย  Polski
Polski  한국어
한국어  Svenska
Svenska  magyar
magyar  Malay
Malay  বাংলা ভাষার
বাংলা ভাষার  Dansk
Dansk  Suomi
Suomi  हिन्दी
हिन्दी  Pilipino
Pilipino  Türkçe
Türkçe  Gaeilge
Gaeilge  العربية
العربية  Indonesia
Indonesia  Norsk
Norsk  تمل
تمل  český
český  ελληνικά
ελληνικά  український
український  Javanese
Javanese  فارسی
فارسی  தமிழ்
தமிழ்  తెలుగు
తెలుగు  नेपाली
नेपाली  Burmese
Burmese  български
български  ລາວ
ລາວ  Latine
Latine  Қазақша
Қазақша  Euskal
Euskal  Azərbaycan
Azərbaycan  Slovenský jazyk
Slovenský jazyk  Македонски
Македонски  Lietuvos
Lietuvos  Eesti Keel
Eesti Keel  Română
Română  Slovenski
Slovenski  मराठी
मराठी  Srpski језик
Srpski језик 








 Online Service
Online Service